by Nick Taylor and Barbara Nevins Taylor
Yes, you can appeal Medicare Part D medication denials and get reversals. It’s slightly time consuming, but if you do it, you have a shot at getting coverage for the prescriptions you need. Why do you need to appeal? You may have gotten a new prescription, or your insurer may have dropped your medication from its formulary, or list of covered drugs, for 2020.
Even if you are not a fighter or a contentious person, this is worth the effort.
Nick uses Vyzulta, a prescription eye drop that reduces pressure in the eye and is prescribed for glaucoma or ocular hypertension. The medication is saving his sight and it’s expensive. He recently paid $412 dollars for a small vial — 5 milliliters, or about a teaspoon — that lasts for perhaps a month. The website of the manufacturer, Bausch and Lomb, points out that there is no generic substitute. His Part D insurance company does not cover the medication because it is not included in its formulary. So Nick thought he’d just have to suck it up and he’s been paying.
But he recently appealed. Here’s how the appeals process works.
1. You have to ask your pharmacist to fill the prescription under your Part D insurance plan. The pharmacist or your plan will give you a formal denial notice.
2. Once you get the denial notice, you must contact your plan and find out how to file an exception request. It’s likely that you can find the form online. Google the name of your plan and formulary exemption form.
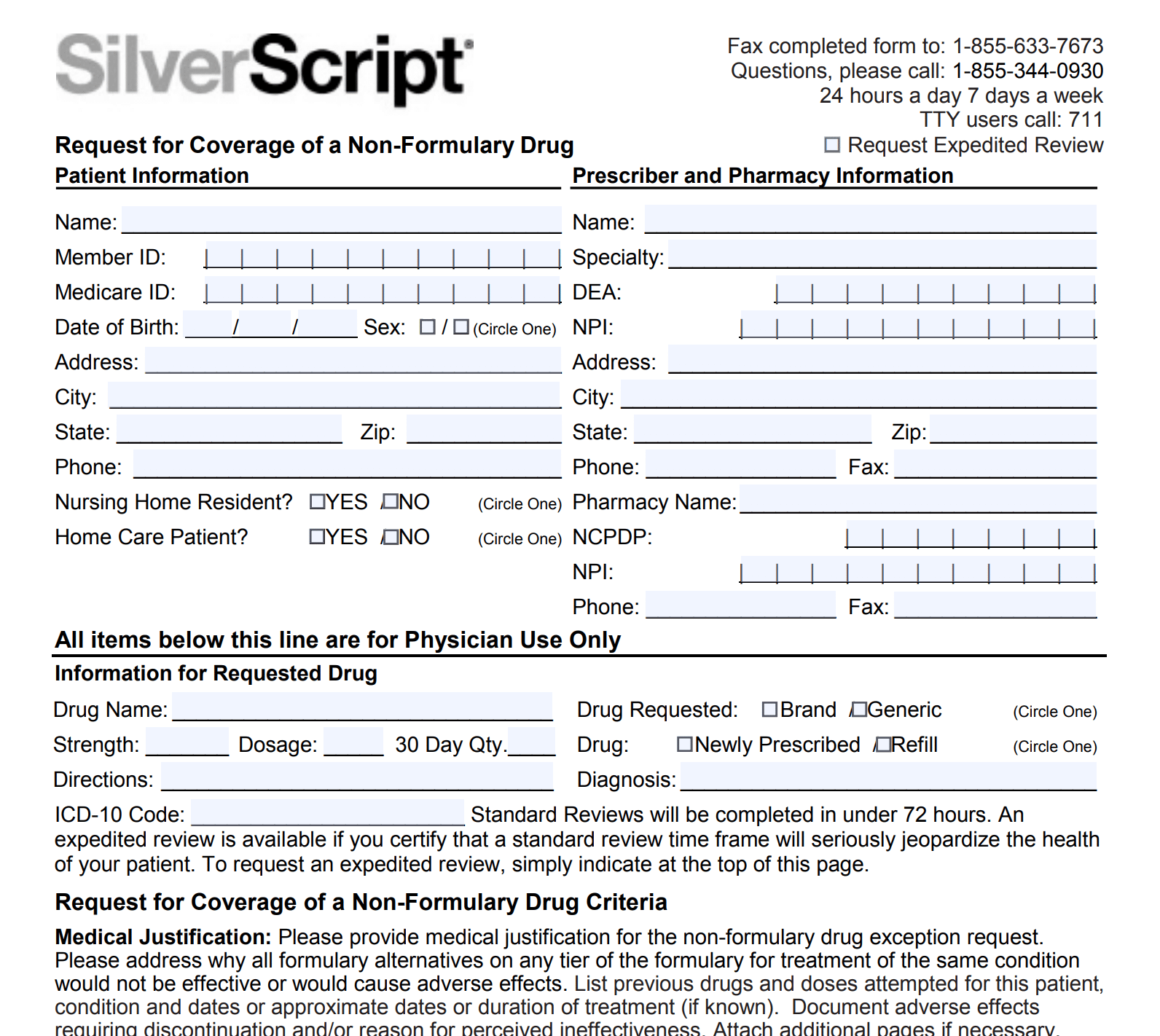
3. Your doctor will have to help out here. She or he needs to fill out the form or write a letter explaining why you need the medication. You should get an answer in 72 hours.
4. You can request expedited exception if your life or health will be threatened if you don’t get the medication. A speeded up request should get an answer within 72 hours.
If they approve it, great. If not, things get a little stickier and you need to do more work.
1. If you get a denial you can appeal to the Independent Review Entity (IRE). That is now a company the Centers for Medicare and Medicaid Services hires to review appeals. That company is now Maximus Federal Services and you can contact them here.
2. Maximus must respond within 72 hours.
3. If they rule against you, you still have the opportunity to request a hearing with an administrative law judge.
Nick didn’t have to take all these steps. He recently changed pharmacies, and his ophthalmologist wrote a new prescription with a note that the Vyzulta was medically necessary. There was no generic and no substitute eyedrop that he can tolerate. SilverScript replied promptly to say they were “pleased to inform you that, upon review of the information provided by you or your doctor, we have approved the requested [Non-Formulary] coverage . . .
The approval will cut his monthly cost almost in half, to $209 for a month’s supply. That’s a big saving, and shows the benefit of going through the appeals process to try to get coverage for the drugs you need.
Let us know about how you deal with drug denials.