What’s the most difficult discussion you ever had? Maybe you haven’t had it yet, and maybe it was about how to treat your parents at the end of their lives.
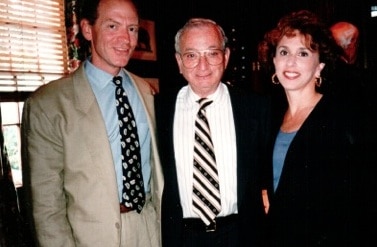
I remember lunch with my dad and stepmother, in Atlanta, long ago. My husband Nick had just published A Necessary End, about taking care of his parents in their final years. And I asked my dad if he had made any plans. He wrinkled his nose, shook his head, ordered a glass of red wine and brushed me off.
But I persisted because my in-laws thought and planned ahead and consequently, doctors, hospitals and nursing homes followed their wishes. They made choices that people abided by and consequently Nick’s parents lived to the end with as much dignity as people could muster in bad circumstances.

My mother-in-law had thoughtfully written everything she wanted down on a yellow legal pad and she and Nick’s dad chose to have living wills that included “do not resuscitate” orders. That meant they did not want extreme measures taken should they begin to slip away.
If they hadn’t thought about this, life support and other measures may have prolonged their suffering and their lives artificially.
My dad had me to talk with. Nick’s parents had him, although they’d already made up their minds. My dad, shortly after our difficult conversation, did have a living will drawn up and so did my stepmom.
But some people find these tough conversations with family members too upsetting and some older people may not have the appropriate people to consult.
That’s why an item about Medicare and end-of-life discussions, buried in a CMS news release, comes as welcome news.
CMS published a proposed rule involving payment to doctors. The new proposal would allow pay for doctors to discuss “advanced care planning” for seniors and other Medicare beneficiaries.
That’s an awfully polite way to say a doctor can talk with you about making plans for your end-of-life care.
CMS carefully says that the proposal follows the recommendations of the American Medical Association “to make advanced care planning services a separately payable service under Medicare.”
These aren’t “death panels,” but discussions everybody needs to have.
The plan will go into effect in the fall after a 60-day comment period.



I am facing pallatve care for lung cancer that has earned me a 100% service/ combat related disability for Agent Orange Exposure on the DMZ in ’68-70. The DMZ was soaking wet with the stuff on the HoChiMinh trail.
I am still left with confusion and Treatment induced Peripheral neuropathy (CIPN) after both my aggressive chemo and followup radiation therapy. I have been clear but start going back for more F#$#$king radiation next month.
I am at the point where I prefer to turn down more chemo which has left me with numb feet and hands, unaware of cuts and bruises. Ripped the baby toe nail now off of both feet and never felt it, but read to be sure to check those tingling, burning toes and fingers for injuries you may not feel
Peter, this is awful, and your choices are difficult. But I gather that you’d rather make them for yourself or discuss them with your family, not just leave them up to someone else. That’s what I hope others will get from the post and your comments. People we love shouldn’t have to guess at the decisions we’d make when time may be short. I hope yours isn’t.